Stop thinking about patient compliance.

One idea that I really dislike is patient compliance. When patients come to see us, they hope the blend of our expertise and experience will help them accomplish their health goals. But that doesn't always mean the patient will follow our recommendations. When that happens, practitioners (myself included!) often get bent out of shape - "why are they even coming to see me if they aren't going to listen to me?!"
Patients may not take their herbs regularly or change their diet or pick up a movement practice or report changing even a single thing about their lives outside of visiting your clinic once a week. Inevitably, you will think to yourself, "If only people just did what I told them to, they would be getting better!"
Feeling like you have the tools that can help someone and watching them not use those tools - the tools they asked for! - can feel frustrating. But, getting stuck in making it about you is a big ego trap. Instead, we need to find new ways to think about our patients' experience and how we can better serve them where they currently are.
There are many reasons why someone may not follow through on your recommendations.
Here are just a few reasons off the top of my head:
- Patients just forgot. (This is especially true if your patient is ADHD.) This can seem inconceivable, but it's very possible. Patients forget to take prescription medication; why would herbs be any different?
- They haven't found a way to integrate the change into their life. For example, finding a time of day that works is a challenge, other life activities conflict, they can't find or afford the food, etc. We will never know this if we don't ask, and this is a perfect chance to help brainstorm with them to see what may work.
- We didn't explain the idea or concept clearly enough.They may be confused about or unsure how to follow our recommendations. Rather than ask for clarification, patients may just opt not to do it.
- We gave them too much to do. Providing an overwhelming amount of information and changes often makes it difficult to know where to start, or to make change seem insurmountable. If it feels too hard to start, they may not start at all.
- Their current habits are serving a purpose. All behaviors have a purpose, even if it may not be a so-called "healthy" choice. This can sometimes be difficult to understand, but I try to see what benefit my patient is getting from the current practice, even if it may not be in the service of their long-term health.
How can someone not be prepared to change?
It may feel logical that patients are ready to change if they are choosing to come to appointments, but I have often found this is not the case. I couldn't figure out how it was possible - people would spend hundreds of dollars (or more!) getting treatments, but still not make any changes in their habits.
Then I came across The Cycle of Change (Prochaska & DiClemente), a useful tool for looking at the change process that patients go through:
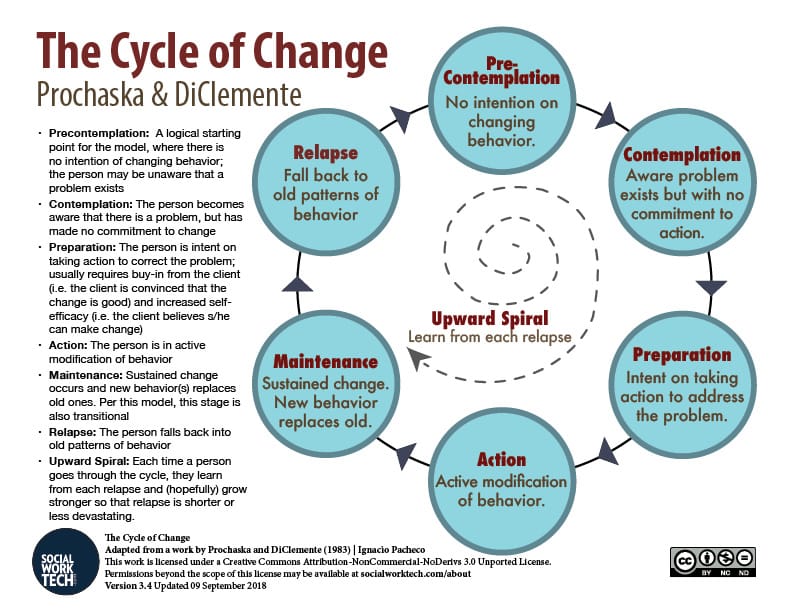
While we may feel that coming to an appointment is an indication of patients being in the Action phase, I think many new patients are more likely to be in the Pre-Contemplation, Contemplation, and Preparation stages.
- They may not know what is wrong, and are seeking out answers (Contemplation).
- Or, they may know what is wrong, but not what to do about it (Preparation).
- We even have patients who are sent to us, either by another health care provider or a loved one, who have no idea there is a problem, and so have no intention of changing (Pre-Contemplation).
New patients are often aware something is wrong when they reach out to a provider - that's why they make an appointment! - but are seeking outside assistance in changing it. They may not be prepared yet to make behavior changes in their own lives yet, but are willing to let others try on their behalf.
There's no shame in that! This is how our medical model is built: we don't feel well, we go to the doctor, they provide a pill (usually), we take the pill, we (hopefully) feel better. Most medical interactions don't involve homework!
As the saying goes, "nothing changes if nothing changes."
Patients first need to understand that change is needed before they can make the change; then they need to understand what to change. It is our job to provide options for them and help them understand why and how our recommendations will help them. We can't skip ahead to the Action phase!
Expecting patients to arrive in our clinic in the Action phase every time is unrealistic; if people knew what they needed to do and were already able to do it, they probably wouldn't need us! Instead of asking why patients aren't following our recommendations, we can ask ourselves which stage our patients are in and, when they're ready, what we can do to help them move to the next stage.